Have you tried RetiCap® N?
RetiCap®N is designed to supplement your diet to help support the eye’s need for specific micronutrients. RetiCap®N food supplement is not a substitute for a varied and balanced diet and a healthy lifestyle!

Diabetic retinopathy is an eye condition that affects individuals with diabetes. It is a complication of diabetes that results from damage to blood vessels at the back of the eye (retina). The condition can arise in individuals with either type 1 or type 2 diabetes.

Diabetic retinopathy is one of the top causes of blindness in the western world, developing in 90% of people with diabetes.
In the UK, it is the leading cause of preventable vision loss or visual impairment. An estimated 4.9 million people are living with diabetes in the UK with increasing numbers predicted. To prevent or manage this eye condition blood sugar, blood pressure and cholesterol levels must be monitored and controlled. Attending routine eye examinations by an eye care professional can help to identify any complications early on.
Diabetic retinopathy can occur as a result of high blood sugar levels. This can affect the retina at the back of the eye. The retina covers the inner surface at the back of the eye and contains a layer of light sensitive nerve cells. These cells are responsible for sending signals to the visual centres in the brain which are then changed into images.
The retina receives a constant supply of blood through lots of tiny blood vessels. However, in cases of diabetic retinopathy, these blood vessels are damaged due to constant high blood sugar levels. If the blood supply is cut off to the retina the eye will try to grow new blood vessels. These new blood vessels don’t form properly and can break and bleed into the eye.
The damage that occurs can progress in stages from mild diabetic retinopathy to severe. The two general categories of diabetic retinopathy are:
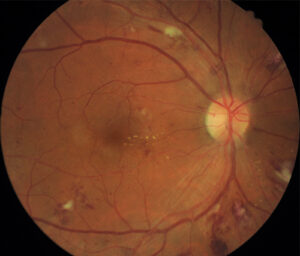
Right eye retina of a patient with diabetic retinopathy
This is the early more common stage of diabetic retinopathy. At this stage, new blood vessels are not developing (proliferating).
Tiny bulges (microaneurysms) stick out of blood vessels and appear as red dots at the back of the eye. These bulges are tiny areas of blood that may leak fluid but may not cause symptoms. Over time more significant changes to blood vessels and bleeding in the eye will result in severe NPDR.
The retina receives a constant supply of blood through lots of tiny blood vessels. However, in cases of diabetic retinopathy, these blood vessels are damaged due to constant high blood sugar levels. If the blood supply is cut off to the retina the eye will try to grow new blood vessels. These new blood vessels don’t form properly and can break and bleed into the eye.
The damage that occurs can progress in stages from mild diabetic retinopathy to severe. The two general categories of diabetic retinopathy are:
At this stage the condition is advanced and the damaged blood vessels have closed off to blood supply. New abnormal blood vessels develop in the retina and can be weak. They can leak into the vitreous (the gel like centre of the eye) and scar tissue can form. This can lead to vision loss due to retinal detachment where the retina pulls away from the back of the eye.
In diabetic retinopathy blood vessels are damaged in the retina along the back of the eye. In some cases, there is damage caused to blood vessels at the centre of the retina (macula). Fluid leaking from blood vessels builds up in the centre of the eye and causes swelling (macular oedema).
In the early stages of diabetic retinopathy, there will not usually be obvious symptoms. One of the earliest signs for diabetic retinopathy is reduced contrast sensitivity.
Contrast sensitivity is the ability to detect the subtle differences between objects and their background. For example, a dark object against a light background (high contrast) is easy to distinguish. If that object gets lighter on a white background (low contrast) it becomes harder to distinguish. Good contrast sensitivity is especially important in low light conditions such as driving at night.
As the condition advances you may start to experience some of the following symptoms. It is important to contact a medical professional to have it checked out.
Early signs of diabetic retinopathy can be picked up during diabetic eye screening. Speak to your GP to find out more about the diabetic retina screening programme.
Any individual with diabetes is at risk of developing diabetic retinopathy but some additional factors can increase this risk. The following are risk factors to consider:
Research is still ongoing in this area to look at the potential for reversing diabetic retinopathy. Currently, treatments are available to slow down and manage the condition to preserve vision. However, the best outcome for treatment depends on detecting and treating the condition as early as possible.
Treatment of diabetic retinopathy depends on how far the condition has progressed. If you have early stage diabetic retinopathy, continued monitoring and management of the condition can help slow the progression.
If your condition is more advanced then immediate treatment is required, some of the available options include:
In some cases, medication is delivered directly into the eye’s vitreous by injection. This can be used for the treatment or prevention of macular oedema where leaking blood vessels cause swelling at the macula. A compound called VEGF helps the growth of blood vessels in the eye. The injections carry anti-VEGF which helps prevent further changes in the eye.
Usually, injections are given once a month to start then less frequently or stopped once vision starts to remain steady. There are possible side effects from the injections including discomfort or irritation and floaters. There are also possible risks including the formation of blood clots.
In cases of advanced retinopathy, lasers can be used. The laser is shone into the eye to treat oedema or abnormal blood vessels in the eye. This treatment will help prevent your vision from becoming worse.
There can be short-lasting side effects for a few hours after treatment including blurred vision, sensitivity to light and discomfort. Some possible risks include reduced night vision, floaters or a small blind spot in the centre of your vision.
Usually, injections are given once a month to start then less frequently or stopped once vision starts to remain steady. There are possible side effects from the injections including discomfort or irritation and floaters. There are also possible risks including the formation of blood clots.
This surgery involves the removal of some of the gel-like substance in the eye (vitreous humour). Surgery may be needed where there is extensive scar tissue or a large amount of blood/fluid in the eye. Usually, you will experience blurred vision after surgery which may take months to return to normal. Some possible risks include the development of a cataract, retinal detachment and fluid build up in the cornea.
Controlling blood sugar levels, blood pressure and cholesterol levels are essential for living with diabetic retinopathy. Several lifestyle improvements can be made including:
Try to do at least 150 minutes of moderate intensity activity during the week. This can be an activity such as a walk each day.
Smoking can increase the risk of complications from diabetes including diabetic retinopathy. If you smoke it’s important to find a quitting plan that works for you.
Attending regular screening such as eye exams will help catch any changes or symptoms in the early stages. Monitoring your health will help reduce the risk of further complications from diabetic eye disease.
If you notice any sudden changes in your vision contact your doctor. Early intervention can help prevent vision loss.
A balanced diet is essential in maintaining a healthy weight and controlling blood sugar. Eating foods rich in nutrients will also help to support eye health. Supplements can also be used to help support your diet and the eye’s need for specific micronutrients.
RetiCap®N is designed to supplement your diet to help support the eye’s need for specific micronutrients. RetiCap®N food supplement is not a substitute for a varied and balanced diet and a healthy lifestyle!
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
More information about our Cookie Policy